Made In Maine: Thoughts on Food, Animals, and Agriculture
Antibiotic Resistance
By Donald E. Hoenig, VMD
Since I began the Made In Maine: Thoughts on Food, Animals, and Agriculture blog a few months ago, I knew that one of these days I had to tackle the complicated topic of antibiotic resistance and antibiotic use in food animals. I haven’t been looking forward to it because, for one thing, I don’t have any amusing or interesting stories to use as a lead in. I do have a good quote, however. A colleague of mine, Dr. Guy Loneragan from Texas Tech, said, “If you think you understand antibiotic resistance, it has not been properly explained to you.” That pretty much sums it up.
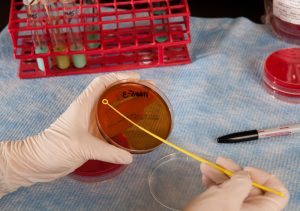 So what’s an antibiotic? An antibiotic is a chemical substance produced by a microorganism that is capable of inhibiting the growth of, or killing, other microorganisms.1 We also use the term to include chemical substances that have been produced synthetically. Most folks have heard of Alexander Fleming who, along with two other scientists, received the Nobel Prize in 1945 for the discovery of penicillin, which ushered in the age of modern antibiotics.
So what’s an antibiotic? An antibiotic is a chemical substance produced by a microorganism that is capable of inhibiting the growth of, or killing, other microorganisms.1 We also use the term to include chemical substances that have been produced synthetically. Most folks have heard of Alexander Fleming who, along with two other scientists, received the Nobel Prize in 1945 for the discovery of penicillin, which ushered in the age of modern antibiotics.
Antibiotics kill bacteria not viruses, which means they can treat things like Staph and Strep infections (Strep throat, for example), but not the common cold or the flu.
According to the Centers for Disease Control, since their discovery in the 1940s, antibiotics have greatly reduced illness and death from infectious diseases. The downside to this is, as antibiotic use has become so widespread, the infectious organisms they’re designed to control have adapted to them (that is, become resistant) greatly reducing their effectiveness. The CDC reports that, in some cases, microorganisms have become so resistant that no antibiotic is effective against them. Antibiotic resistance is one of the world’s most pressing public health problems.2
What’s being done to address this scary situation? On the human side of the equation, physicians will only prescribe antibiotic treatment when it’s likely to be of benefit to the patient and will try as much as possible to use a drug which targets the likely bacteria causing the infection. They will usually not provide an antibiotic for a viral infection such as colds or the flu.
What can you do? Take the antibiotic exactly as prescribed by your health care provider, don’t skip doses, and complete the course of antibiotics even if you start feeling better. Stopping treatment too soon may allow some bacteria to survive and re-infect.
What about antibiotic use in farm animals? It’s difficult to obtain exact figures about how much antibiotic use there is in food-producing animals in this country, but the figure is high. Antibiotics are given to animals either for therapeutic reasons, i.e. to treat, prevent or control a disease, or for non-therapeutic reasons. Antibiotics used non-therapeutically (also called growth promotion or feed efficiency) are administered in either the feed or the water and can be used without the consultation of a veterinarian.
Veterinarians and farmers who use antibiotics are required by law to withhold meat and/or milk for specified periods of time to assure that the food supply stays free of antibiotic residues.
In December 2013, the U.S. Food and Drug Administration announced new voluntary guidelines in its policy regarding non-therapeutic uses of medically important antibiotics in food-producing animals. The FDA stated that it considers the non-therapeutic use of antibiotics in feed and water to be “injudicious” and will be phasing out these uses within three years. Additionally, the FDA will now require veterinary oversight of all these antibiotics, essentially requiring a veterinary prescription for their use.
If you want to learn more, the Maine Organic Farmers and Gardeners Association is holding a teach-in on this topic Saturday, September 20 at 2:00 PM at the Common Ground Fair in Unity Maine. I’ll be on the panel along with Dr. Stephen Sears, former Maine State Epidemiologist; Jennifer Obadia, Ph.D.; and Alice Percy, an organic farmer from Whitefield. Hope to see you there.
1http://medicaldictionary.thefreedictionary.com/antibiotic
2http://www.cdc.gov/drugresistance/about.html
Dr. Hoenig retired as the Maine State Veterinarian in 2012 and, after completing a year-long Congressional Fellowship in Sen. Susan Collins’ office in Washington DC last year, in January 2014 he started working as a part-time Extension Veterinarian for University of Maine Cooperative Extension.
Dr. Hoenig invites you to submit questions and comments to dochoenigvmd78@gmail.com. Answers to selected questions will appear in future blog posts.
