Eliminating Chronic Disease Using a Farmbased Approach: Caseous Lymphadenitis (CL)
SARE Farmer Grant Final Report 2014
By Anne Lichtenwalner DVM Ph.D., University of Maine Cooperative Extension, and Animal and Veterinary Sciences
CL: What is it?
- “Cheesy gland”: Chronic bacterial infection Corynebacterium pseudotuberculosis
- Stays in the immune system
- May cause skin or internal abscesses
- Can be spread from animal to animal:
- Must have skin penetration
-

The location of lymph nodes on a goat. Persistent in the environment
- Use antibody response to test for the presence of bacteria in unvaccinated animals
- Vaccines are available; not highly effective
Corynebacterium pseudotuberculosis: lymph nodes
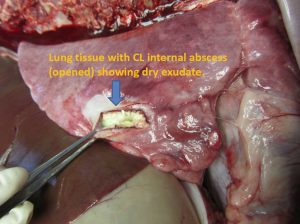
- External: Firm, dry abscesses- slow to develop
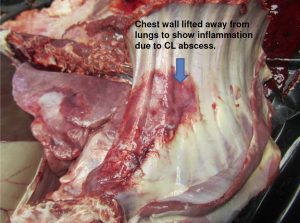
- Internal: Weight loss, coughing
CL: Internal abscesses (goat at necropsy)
CL: How contagious is it?
Transmissibility
- Direct inoculation of bacteria into new host
- Cut or ulcer, contact with exudate
- Bites from flies that have contacted exudate
- Rubbing on a tree, etc. that has exudate on it
- Inhalation of infected secretions
- Sheep with bronchial lymph node abscesses: coughing
- Milk?
- If mammary lymph infections present
- See more recent info (below)
Treatment
- Vaccines or antitoxins:
- Don’t prevent or cure, but may decrease abscesses
- Immune clearance ineffective
- Toxins overcome normal immune defenses
- “Hides out” inside cells
- Uptaken by macrophages; survives and is spread to lymph nodes
- Antibiotics
- In vitro, many are effective
- In vivo, nothing works: food animal limitations re antibiotics
- Rifampin with tetracycline was useful in early infection
Sources:
Judson et al, 1991. Veterinary Microbiology 27(2): 145-150.
Senturk and Temizel, 2006. Veterinary Record 159(7): 216-217
CL: How long does it last on my farm?
Non-spore former, but environmentally stable
- C. pseudotuberculosis wasn’t killed by 4 months in soil samples containing exudate from CL abscesses, and after 11 months in sterilized soil samples (40º F, 72º F, 98 º F and ambient conditions).
- C. pseudotuberculosis was killed after 3 hours in chlorinated tap water but could survive up to 70 hours in distilled water.
- Disinfectants: many are effective against CL after a thorough cleaning of surfaces. However: rough surfaces such as wood may be impossible to disinfect.
 CL: Can I detect or prevent it?
CL: Can I detect or prevent it?
Detection
- Exposed animals: PLD antibodies
- Test-based on detecting antibodies
- “Seropositives” carry the bacteria
Prevention
- Vaccines not 100% effective
- Boosters, accurate records needed
- Vaccine will NOT cure, only help prevent abscesses
- Using vaccine creates “seropositives”
- Testing and culling seropositives: best method
- But will this work for all farms?
Trial Methods
SARE Grant: CL in Sheep
- Visit farm: use farm vet if possible
- Test sheep: 0 and at least 60 days
- Initial SHI tests were done by Washington State University
- Report results (farm ID confidential)
- Consultation
- Biosecurity
- Tailor methods to farm type
- Survey
- SHI test method developed at UMaine lab in Orono
- Supports local industry
- Create easier access to vigilance methods
- Validate CL-free status for producers
Farm types tested
- Breeds: Many
- Products: Fiber, meat, milk
- Biosecurity: Varied greatly
CL status
- 8 of 17 had positive animals at first test (47%)
- 22% of 705 sheep tested at least once were CL+
- 8 of 9 negative farms stayed negative (1 didn’t retest). Closed herd and good biosecurity essential
- Inability to run test locally interfered with outcome
- At follow-up, most of the positive farms had culled or isolated positive animals
Biosecurity: example (Farm 2)
- Breeding for fiber and meat: Animals may travel off farm: limited or no quarantine
- Tested “home” animals: all neg.
- Tested “returned” animals: 1 pos.
- Retested “home” animals: new positive
Followup: culled all positives, implemented quarantine procedures for returning animals
Trial Results
Farmer compliance
- All farmers directly contacted said they would cull
- Follow-through really varied. “Favorites” or great producers were unlikely to be culled.
- Most were unwilling to replace wooden feeders or other areas where CL transmission likely.
- Most thought their biosecurity was excellent
- All were highly concerned and involved in the success of their flocks
- Some of the 17 farms had camelids; none had goats
Farmers resented “buying” chronic disease
- “Do unto others” was a strong motive
Conclusions
- Prevalence higher than expected
- Does being CL-free add to value?
- “Caveat emptor”: Selling CL free breeding stock=value
- Other species affected: goats, camelids
- Be careful of guard animals: need testing, too
- Farm type dictates whether vaccination ok
- Reluctance to cull is common
- Vaccination takes away possibility of testing
- No strategy works longterm without culling
- Biosecurity and determination dictate whether disease-free status is achievable
Outcomes
- Awareness of CL increased
- Added value of CL-free status
- Biosecurity templates in development
- Google Earth model may help communications about farm layout and biosecurity
- SHI method now in Orono on a research basis
- Project continuing studying goat dairies in 2014-5
- Sheep testing available in 2015 if serum samples can be collected/shipped to UMAHL (no charge for testing)
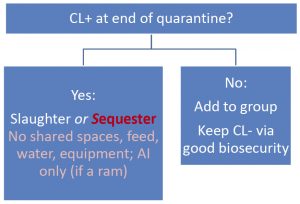
- Decision Tree: Start by knowing your status
- Assess the cost of CL-free status for your farm
- May not work for everyone
Outcomes: Recommendations
- Know the CL status of your flock: retest as needed
- Maintain closed flock/herd with high biosecurity
- Notify visitors about biosecurity
- Inform shearers about biosecurity
- New or returning animals:
- Don’t immediately mix with “home” flock
- “nose to nose H quaranIne”
- CL test immediately at entry and prior to release from quarantine (2 mo. later)
- If positive, cull or sequester positives
- Don’t immediately mix with “home” flock
» Retest exposed animals at 2 months: cull if +
» Keep quarantined until all negative for CL at 2 consecutive tests 2 months apart
Outcomes: Decision Tree
Outcomes: Decision Tree
Impacts
- Stopped CL on several farms
- Estimated 20% improvement in fiber yields
- Potentially reduced carcass condemnation
- Outreach to SR vets
- Free testing may enhance communications
- Help establish VCPR with farmers
- Farmer-to-farmer:
- Added value of CL-free stock
- Building biosecurity awareness
- Students
- projects and experience
Recent Undergrad Student Theses on SR
- Edith Kershner: Case study of sheep farms with or without CL.
- Abigail Royer: Detecting CL using complete blood counts.
- Amy Fish: Evaluating macrophage responses to CL.
- Rachel Chase: Evaluating neutrophil responses to CL.
- Cassandra Karcs: CL prevention in small ruminants.
- Hallie Lipinski: CL and its connection to milk.
- Anna Desmarais: Selenium and footrot prevalence.
- Alden West: Composting effects on coccidia.
- Alexandra Settele: Anthelmintic resistance in H. contortus
- Amanda Chaney: Identification of internal parasites of sheep and goats
- Caitlin Minutolo: Effect of age on susceptibility to ovine footrot.
- Nicole Maher: CL webinar for producers
- Casey Athanas: Pedigree analysis to help eradicate footrot.
- Katrina Glaude: Should sheep with footrot be culled?
- Kayla Porcelli: Biosecurity survey for footrot positive farms
- Marie Smith: Pasture management to control parasites in small ruminants.
References
- Sheep and Goat, Wool and Mohair: 1982. Research reports, Texas A and M University.
- Augustine JL and Renshaw HW. Longevity of C. pseudotuberculosis in six Texas soils. P 102
- Augustine JL, Richards AB, Renshaw HW. Persistence of C. pseudotuberculosis in water from various sources. P 104.
- Assis RA, Lobato FCF, Martins NE, et al. Clostridial myonecrosis in sheep after caseous lymphadenitis vaccination. The Veterinary Record 2004;154:380-380.
- Paton MW, Walker SB, Rose IR, et al. Prevalence of caseous lymphadenitis and usage of caseous lymphadenitis vaccines in sheep flocks. Australian Veterinary Journal 2003;81:91-95.
- Fontaine MC, Baird G, Connor KM, et al. Vaccination confers significant protection of sheep against infection with a virulent United Kingdom strain of Corynebacterium pseudotuberculosis. Vaccine 2006;24:5986-5996.
- Baird GJ, Malone FE. Control of caseous lymphadenitis in six sheep flocks using clinical examination and regular ELISA testing. The Veterinary Record 2010;166:358- 362.
- Washburn KE, Bissett WT, Fajt VR, et al. Comparison of three treatment regimens for sheep and goats with caseous lymphadenitis. Journal Of The American Veterinary Medical Association 2009;234:1162-1166.
Acknowledgements
- Collaborating Farmers of Maine
- Collaborating Veterinarians:
- Drs. Becky Myers Law and colleagues
- Dr. Tammy Doughty
- Dr. Don McLean
- Dr. Beth McEvoy
- NE SARE: Carol Delaney
- Extension colleagues: Richard Brzozowski and Donna Coffin
- Technical/lab assistance:
- Edith Kershner, Anne Ryan, Hallie Lipinski, Abbie Royer
- Ann Bryant
- University of Maine Cooperative Extension
- University of Maine School of Food and Agriculture